Printer-Friendly PDF | Large-Print PDF
Drive-thru medical sites are one way that hospitals and health departments provide intermittent medical services (such as administering the flu vaccine) with greater ease and/or safety for their patients. Typically consisting of pop-up tents and traffic cones, these temporary sites may be located in a parking lot at the hospital or a retail store or in a state fairground.
The sites are especially useful for medical testing during times of an outbreak since keeping patients in vehicles can help to minimize exposure to a contagious disease. In these cases, the patient’s vehicle may be approached by a medical provider who is wearing personal protective equipment (e.g. face mask, gloves, and a smock), and the patient may be instructed to lower their window to allow a 4-inch gap, through which the provider communicates with, performs the test on, and exchanges written information with the patient.
Whether these drive-thru medical services are funded and/or operated by the state, county, or city or a private business, the Americans with Disabilities Act (ADA) requires that the services are accessible to people with disabilities. This fact sheet lists considerations and strategies to promote accessibility at drive-thru medical sites, including those sites where patients may be asked to exit their vehicles.
“Nothing about us without us”
Involve the disability community in planning and implementation. Centers for Independent Living are locally-based organizations, staffed by people with disabilities, that can offer guidance and support to ensure programs and activities are readily useable by and accessible to people with disabilities. Disability consumer groups, including those listed in the “Resources” section of this fact sheet, can provide practical information on how to remove barriers and provide access in specific situations.
Train staff on disability etiquette
There are a number of disability language and etiquette resources, including those listed at the end of this document, which emphasize the following pointers:
- Communicate with the client directly
- Use plain language when explaining things to clients, whether spoken or written
- Allow extra time, and don’t rush or interrupt the patient
- For people who are blind or have low vision, ask permission to touch the person, and let them know when you’re reaching out to them and handing them something. Staff can also learn human guide techniques in order to assist someone from their vehicle to another onsite location, if applicable.
Accommodation requests
- Ask patients to state their accommodation needs during the registration phase and before their arrival to the site
- If you expect patients to register using a website, ensure that the website is accessible. Offer to take accommodation requests by phone and email.
Wheelchair-user access
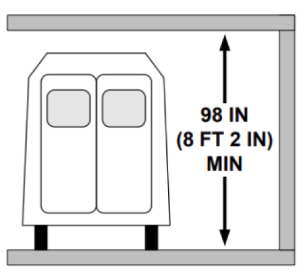
- Minimum clearance for wheelchair-accessible vans to approach and pass through the site is 8 feet and 2 inches high (see graphic)
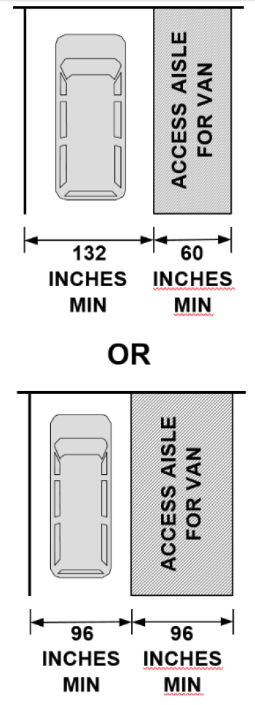
- In order for patients who use wheelchairs to exit their vehicles at the drive-thru site (if instructed to do so), there needs to be an access aisle (clear space) alongside the vehicle. The access aisle must be at least 60 inches wide if the lane is 132 inches wide, and the access aisle must be at least 96 inches wide if the lane is 96 inches wide. (see graphic)
Service animals
Under the ADA, service animals are defined as dogs (or miniature horses) that are specifically and individually trained to perform a task or tasks for the person with a disability. These animals are permitted to accompany the person with the disability anywhere that patients are allowed to go so long as the animal doesn’t pose a direct threat to the safety of the person or others. Therefore, patients who are instructed to exit their vehicles and/or travel to another location in order to receive services elsewhere must be allowed to take their service animals with them.
Effective communication
Staff communication with people who have disabilities must be as effective as it is for people without disabilities. This includes efforts to notify those who are eligible about the opening of drive-thru medical sites.
For people who are deaf or hard of hearing:
- Covering providers’ mouths with masks could hinder some Deaf patients who use lip-reading as part of their overall communication strategy. This will include many older people with age-onset hearing loss. Be prepared to communicate in different ways.
- If onsite ASL interpreters don protective smocks and gloves, give them gloves that provide high color contrast against the smocks (e.g. if the smocks are white, use black gloves)
- Use standard questions on a form (in bold, large font) that testers can point to
- Use printed instructions and descriptions of procedures (swab, etc.) so that people are prepared
- For written communication, testers can use a small dry-erase board, which can be disinfected
- Consider having small pads of paper and pencils for patients to use (and keep)
- Use charts with graphics for visual communicators
- Encourage testers to be as gestural as possible
- Offer assisted listening systems and devices. A mobile device, such as a smart tablet, can be used for communication. Use a rugged case to protect the device from falls, and use a bio-bag and disinfection measures to prevent cross-contamination. The device can also be mounted on a stand with casters to roll the device to the patient’s window and to minimize handling of the device itself.
- Set up a communication system at the site so that drivers with ASL needs can be connected with the onsite ASL interpreter with little delay. Drivers who need ASL can be allowed to skip initial checkpoints in order to be expedited to the onsite ASL interpreter.
- Video remote interpreting (VRI) is an option if an in-person ASL interpreter cannot be scheduled
- Information on VRI resources, communication apps, and other communication strategies can be found at “COVID-19: Deaf and Hard of Hearing Communication Access Recommendations for the Hospital”
For people who are blind or have low vision:
- State your name and title clearly, and repeat this introduction if there are multiple personnel involved so that the patient can identify who is talking to them
- Verbally describe each step of the procedure, using specific directional words like “left” and “right,” etc. instead of “here” and “there”
- Provide written materials in high-contrast large print, Unified English braille, and as text-only files that can be emailed to the person
- If written materials are laminated or plastic, use low-glare coating whenever possible
- Provide adequate, dimmable, directional lighting for all items that require close-up reading
- Offer to read documents aloud to the person
- Offer to handwrite for the person to fill out a form, etc.
- To mark a signature area, use a plastic signature guide, which can be disinfected (see graphic)
Additional measures for greater accessibility
Consider if it would be safe and achievable to implement any of the following ideas (as applicable) for even greater accessibility of service:
- A TV screen at the entry to the site plays a video instructing drivers on where to go and what to do. The video is in all formats –plain language, audio-described, with ASL and captioning.
- Strong WIFI signal, to which patients can connect their communication devices and other assistive technology
- Onsite services provided to city bus, paratransit, and senior shuttles passengers (decide if passengers can remain in the vehicle or must exit the vehicle)
- Walk-up services for people who cannot arrive onsite aboard a vehicle. For example, some people who are blind would walk to a temporary medical site, especially if drivers are scarce.
- Self-administered medical test kits mailed to people who are unable to leave their homes or arrive by vehicle to the drive-thru site. For people who are blind or have low vision, test instructions would need to be available in alternative formats (e.g. large print, braille, audio file, or video conferencing); and it would be helpful to provide self-addressed, postage-paid return packaging or a variety of ways to submit the kits to the lab.
Resources
COVID-19: Deaf and Hard of Hearing Communication Access Recommendations for the Hospital, National Association of the Deaf
Washington Council of the Blind (WCB)
Center for Independence (CFI), Todd Holloway, IL Educator
Washington State Independent Living Council’s Coalition on Inclusive Emergency Planning (CIEP), James House, Disability Integration Manager
FEMA Office of Disability Integration and Coordination
Deaf/Hard of Hearing/Deaf-Blind Medical Placard, Telecommunications for the Deaf INC. (TDI)
List of Technology Tools (for people with hearing disabilities), Telecommunications for the Deaf, INC. (TDI)
COVID 19 Picture Communication Board (Powerpoint file), University of Colorado Denver, Center for Inclusive Design and Engineering
Human Guide Technique, Northwest ADA Center
Respectful Interactions: Disability Language & Etiquette, Northwest ADA Center
Guide to Interacting with People Who Have Disabilities, US Dept of Homeland Security
Tips for Effectively Communicating with the Whole Community in Disasters, US Dept of Homeland Security
University of Washington’s Accessible Design and Innovative Inclusion
Emergency Preparedness Publications and Resources, Pacific ADA Center
Accessibility Checklists, Northwest ADA Center

The Northwest ADA Center is a member of the ADA National Network. This fact sheet was developed under grant from the Administration for Community Living (ACL), NIDILRR grant #90DPAD0002. However, the contents do not necessarily represent the policy of the ACL, and you should not assume endorsement by the federal government.
Alternate formats available upon request.